Transcranial Magnetic Stimulation Vs. Electroconvulsive Therapy: Is There A Difference?
When it comes to depression treatment, various options exist, each with its own benefits and considerations. Transcranial Magnetic Stimulation (TMS) and Electroconvulsive Therapy (ECT) are two distinct approaches that have gained recognition for their effectiveness in managing treatment-resistant depression.
In this article, we will explore the differences between TMS and ECT, shedding light on their mechanisms, side effects, and overall efficacy. By understanding these contrasting therapies, individuals can make informed decisions regarding their depression treatment journey.
The Basics of Transcranial Magnetic Stimulation
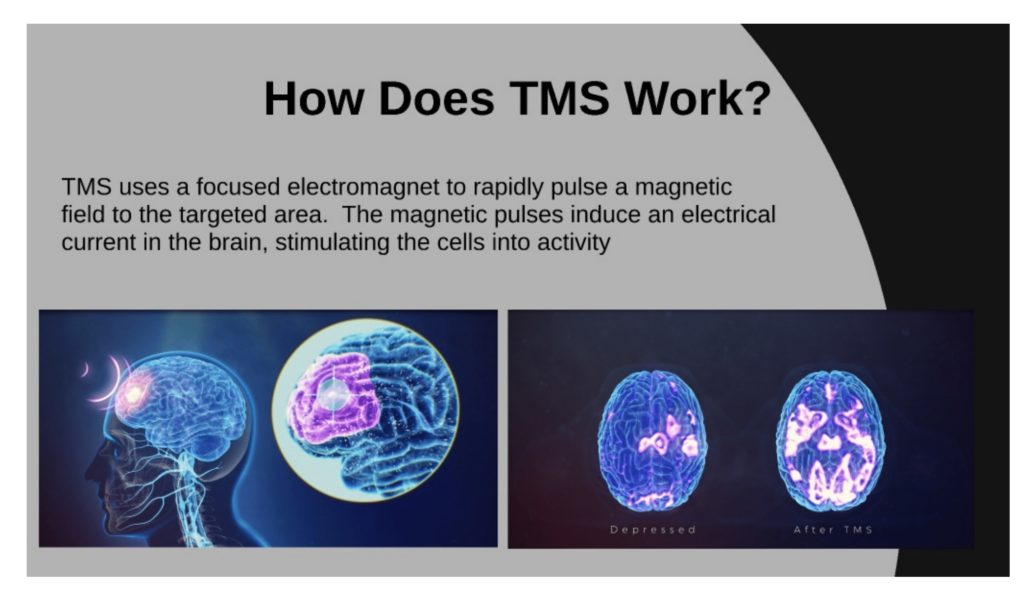
Transcranial magnetic stimulation stimulates particular brain areas linked to depression by using magnetic fields. TMS is a minimally invasive technique that involves pressing a coil against the scalp and delivering magnetic pulses through it. These pulses aim to activate or modulate the neural circuits involved in mood regulation. TMS is typically administered on an outpatient basis and does not require anesthesia, allowing individuals to resume their daily activities soon after the treatment session.
The Basics of Electroconvulsive Therapy
Electroconvulsive Therapy, on the other hand, is a more invasive approach that involves the controlled induction of seizures to alleviate severe depression. During ECT, an electrical current is passed through the brain, triggering a brief seizure under general anesthesia. ECT sessions are conducted in a hospital setting and require careful monitoring by a trained medical team. ECT is often reserved for individuals with treatment-resistant depression or those who cannot tolerate other forms of treatment.
Efficacy and Treatment Course
Both TMS and ECT have shown efficacy in treating depression; however, their response rates and treatment courses differ. TMS is typically administered as a series of sessions over several weeks, with patients undergoing daily treatments.
The response to TMS may be gradual, with improvement reported over time. ECT, on the other hand, often yields faster results, with significant improvement observed after just a few sessions. ECT is usually administered two to three times a week for a few weeks, followed by maintenance treatments as needed.
Side Effects and Safety Considerations
TMS is generally well-tolerated, with minimal side effects. Some individuals may experience mild scalp discomfort or headache during or after the procedure, but these effects are typically temporary and resolve on their own. ECT, however, may be associated with more pronounced side effects. These can include memory loss, confusion, and headaches. It is important to discuss potential risks and benefits with a healthcare professional when considering ECT as a depression treatment option.
Anesthesia and Hospitalization
TMS does not require anesthesia or hospitalization, making it a more convenient and accessible treatment option for many individuals. The non-invasive nature of TMS allows patients to drive themselves to and from treatment sessions, minimizing disruptions to their daily routines. ECT, in contrast, requires general anesthesia and necessitates hospital visits, potentially impacting work or personal commitments.
Treatment Considerations
TMS and ECT have different considerations based on individual needs and preferences. TMS is well-suited for individuals seeking a non-invasive approach with minimal side effects and the ability to maintain their daily activities. ECT, on the other hand, may be recommended for individuals with severe depression or those who have not responded well to other treatments. The decision between TMS and ECT should be made in consultation with a healthcare professional, taking into account the severity of the condition and individual circumstances.